60% of all hospital patients
are not continuously monitored.
Frequent spot checks leave patients unmonitored for 96% of their hospital stay.
(AHA Database, 2013) , (Weinger MB and Lee La. No patient shall be harmed by opioid-induced respiratory depression. APSF Newsletter. Fall. 2011.)

Detect deterioration in real-time = provide rapid proactive responses for early intervention.
Monitoring of motion, resting heart rate and respiratory rate of a patient allows recognition of changes that may indicate onset of various CRD/CVD and other preventable forms of deterioration.
Why continuous monitoring matters
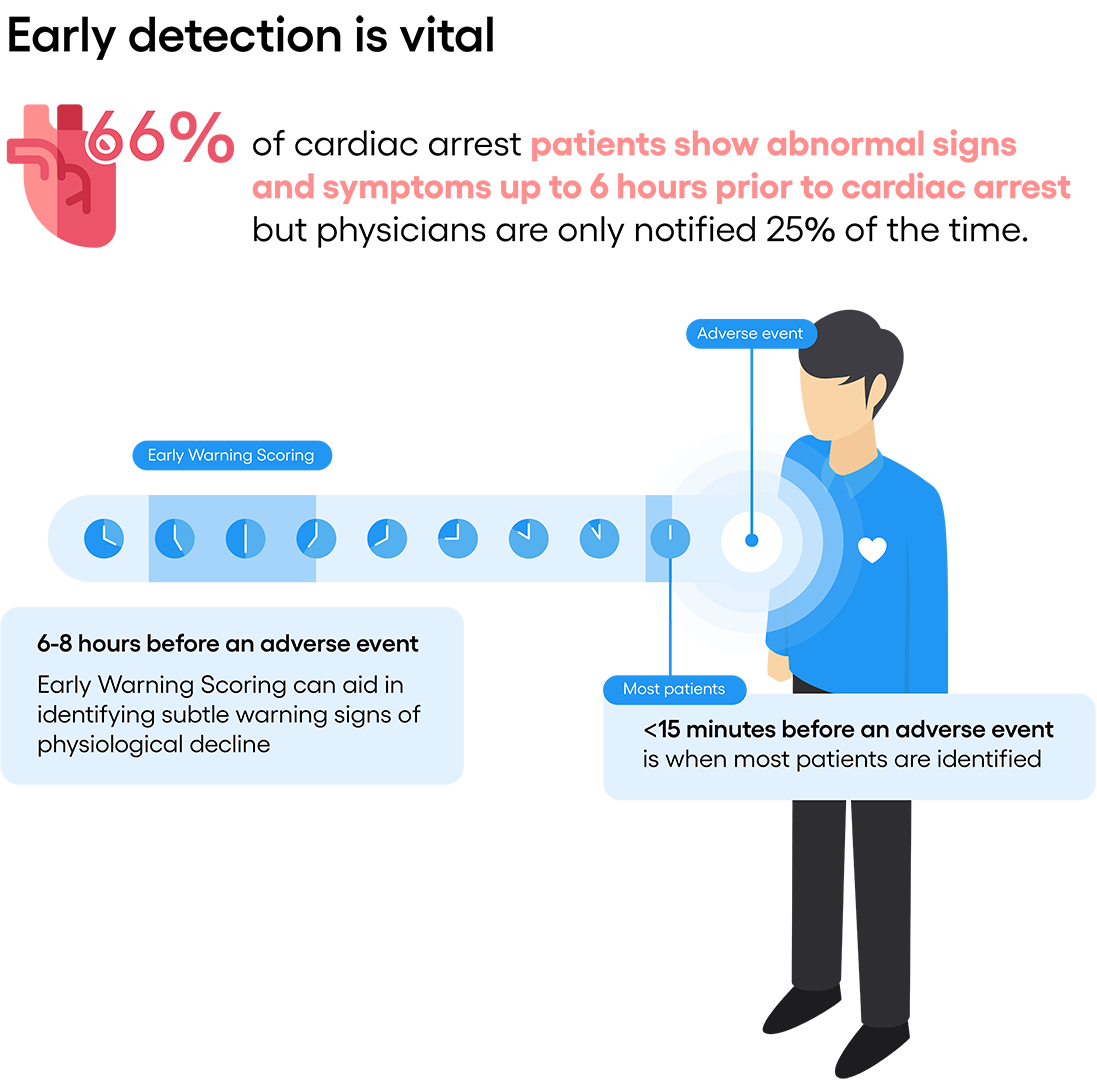
- Most critical events are preceded by warning signs 6 to 8 hours prior to an event. Respiratory rate is the best early indicator of patient deterioration.1
- 3-5 more breaths/min is an early sign of respiratory distress.2
- Respiratory rate is a predictor of cardiac arrest in hospital wards even the 1st time it reaches 27 breath/min. within a 72 hr. period.3
- When respiratory rate is 25-29 breaths/min,, mortality rate is 21%.4
SpO2 vs. Respiratory Rate. Why RR is often dismissed in hospitals today:
The recommended method for measuring respiratory rate (RR) is counting breaths for 60 seconds using a timer manually by a nurse during a spot check on the patient. This method is not efficient in a busy clinical setting. Also, the fact that the nurse is “looking” at the patient for 20-60 seconds may adversely affect the accuracy of the measurement as it makes certain patients uneasy. 27.4% of nurses indicated that they make quick estimates of RR.(1) Respiratory Inductive Plethysmography (RIP) and Co2 masks are sometimes used, but they are uncomfortable and costly. Obtaining RR reading once every few hours from this method is not consistent and reliable.
Therefore, a survey of general care nurses and clinicians claimed that 60% of them relied on Oxygen saturation (SpO2) data to evaluate respiratory dysfunction.(2) Respiratory rate was the only parameter recorded less than 50% of the time.(1)
Created by Nucleus Medical Media.
COVID19 example
When the virus attacks the lungs, inflammation in the lower respiratory tract can lead to distress. It also causes the lungs to carry less air, thus less oxygen each and every breath. The lung starts to compensate by breathing more (increase breath/min) and the heart also tries to help by pumping more blood (increase in BPM). If and when this is not enough to bring enough oxygen to the body’s core organs, blood oxygen levels (SpO2) starts to fall. Therefore, SpO2 data is actually a much slower indicator of deterioration when compared to RR and RHR data.
Problems addressed by XK300
- 63% of preventable deaths are attributed to failure to rescue by a registered nurse or physician due to inability to monitor continuously.5
- 60% of all hospital patients are not continuously monitored. Frequent spot checks leave patients unmonitored for 96% of their hospital stay.6
- Respiratory rate is often measured inconsistently, incorrectly and infrequently at the hospital as it is mostly done manually (visual reading) every 4-8 hours.
Unfortunately, however, respiratory rate is often measured inconsistently, incorrectly and infrequently.
Provide sustainable, quality care in general care while creating a better working environment for your nurses and staff.
Continuous and automatic vital sign monitoring of patients can help end preventable deaths and provide more timely care. Time pressures and work interruptions contribute to missed respiratory rates. 7
High patient turnover, or patient inflow and outflow generated by admissions, discharges and transfers is a critical factor increasing nurse workload. As patient turnover increases, failure-to-rescue also increases. High patient turnover is associated with increased mortality.

100 Hospital Bed Scenario
Fully automated, continuous and contact-free.
No staff intervention or patient participation required.
Current method:
Spot-check every 4 hours = 6 spot checks per 24 hours.
Average 5 minutes per visit = 30 minutes per day per bed.
100 beds = 6 x 100 visits = 600 visits per day or 50 hours.
With Xandar Kardian XK300:
24 hour continuous monitoring with customized alerts.
100 beds = 0 or minimal spot checks per day.
Unfortunately, however, respiratory rate is often measured inconsistently, incorrectly and infrequently.
Real-time Notification via Cloud Dashboard and Mobile App Push Alert.
Secure, HIPAA compliant cloud servers can receive and store health data of residents with the ability to integrate patient EHR data. Furthermore, real-time alerts can be pushed out to various tablets, smartphones or even wearables, making it easier for staffs to get alerts wherever they are.
Get historical data over hours, days, weeks or months which can be provide important information about their overall respiratory and cardiovascular health status. In fact, if the resident qualifies for certain conditions, the entire system can be reimbursed through CPT CODE 99454. Contact us for more details.
1. Al-Qahtani S, Al-Dorzi HM. Ann Thorac Med. 2010;5(1):1–4
2. Field D (2006) ‘Respiratory care’. In: Sheppard M, Wright M eds. Principles and practice of high dependency nursing 2nd edn. Bailliere Tindall, Edinburgh
3. Fieselmann JF, Hendryx MS, Helms CM, et al. Respiratory rate predicts cardiopulmonary arrest for internal medicine patients. J Gen Intern Med 1993; 8: 354-360.
4. Goldhill DR, McNarry AF, Mandersloot G, et al. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia 2005; 60: 547-553
5. HealthGrades, Inc: Third Annual Patient Safety in American Hospitals Study. April 2006
6. AHA Database, 2013) , (Weinger MB and Lee La. No patient shall be harmed by opioid-induced respiratory depression. APSF Newsletter. Fall. 2011.
7. (Ansell, H. et el. Why don’t nurses consistently take patient respiratory rates? Br J Nurs. 2014 Apr 24-May 7;23(8):414-8).
Copyright ©2022 Xandar Kardian Inc. All Rights Reserved.
Let's find a solution
Find out how radar technology can benefit your healthcare operation